Peri-implantitis is a bacterial infection that affects the soft and hard tissues surrounding dental implants, leading to inflammation and eventual implant failure. Treatment options for peri-implantitis have been extensively studied in recent scientific and clinical research. This blog post will explore the latest research findings and effective treatment options for peri-implantitis.
Diagnosis
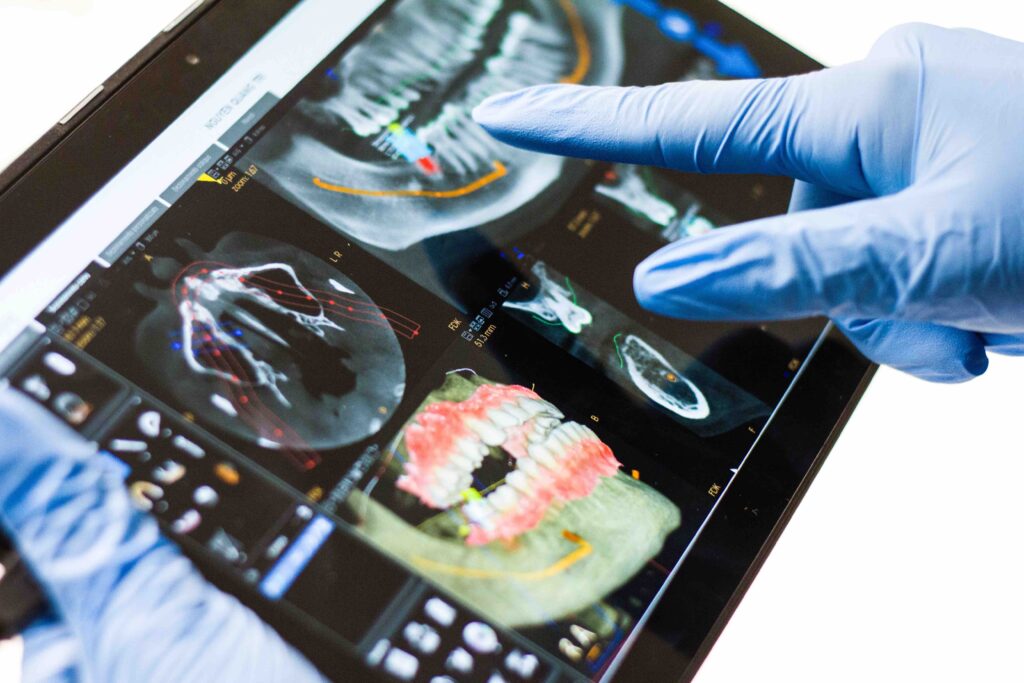
Diagnosis of peri-implantitis involves a combination of clinical and radiographic assessments. Some common symptoms include bleeding on probing, suppuration, and increased probing depths. Radiographic evidence of bone loss around the implant is also indicative of peri-implantitis. New technologies, such as 3D imaging, have also been introduced to improve the accuracy of diagnosis.
Prevention
Prevention is critical to avoiding peri-implantitis. Good oral hygiene and regular professional dental cleanings are crucial to preventing bacterial colonization and inflammation around the implant. Additionally, patient education on implant maintenance and regular check-ups is essential in preventing peri-implantitis.
Treatment
Several treatment options are available for peri-implantitis, including non-surgical and surgical approaches.
Non-surgical treatment: Non-surgical treatment options for peri-implantitis include mechanical debridement, chemical disinfection, and laser therapy. Mechanical debridement involves the removal of plaque and calculus using hand or ultrasonic instruments. Chemical disinfection with antiseptics or antibiotics has also been used to control bacterial infection. Laser therapy, specifically diode laser, effectively reduces inflammation and promotes bone regeneration.
Surgical treatment: Surgical treatment options for peri-implantitis include open flap debridement, bone grafting, and guided bone regeneration. Open flap debridement involves surgically accessing the implant and debriding the infected tissues. Bone grafting and guided bone regeneration are aimed at promoting bone regeneration around the implant.
Combination therapy: Recent studies have shown that a combination of non-surgical and surgical treatment modalities may provide better outcomes for peri-implantitis. Mechanical debridement, topical antibiotics, and surgical treatment significantly improved clinical and radiographic outcomes.
Conclusion
Peri-implantitis is a challenging complication that requires early diagnosis and prompt treatment. The latest scientific and clinical research has provided new insights into diagnosing, preventing, and treating peri-implantitis. A multidisciplinary approach involving the dentist, hygienist, and patient is crucial for successfully managing peri-implantitis. With proper diagnosis, prevention, and treatment, peri-implantitis can be managed effectively, leading to improved long-term implant success.